Osteoarthritis of the thigh joint is a chronic, progressive pathology in which degenerative-dystrophic processes occur in the area of the pelvic bone joints. To be more precise, there is a destruction of the hyaline cartilage lining the femoral head and the acetabulum, the surfaces of the pelvic bones that are in contact with each other.
The second name of the pathology is coxarthrosis of the hip joints.
Osteoarthritis of the hip joints: features of the disease
Most often, first-hand knowledge of what coxarthrosis is is for older people, mainly women, who are at risk of developing pathology after 45 years. Such a selective manifestation of pathology comes from the specifics of the pelvic bone structure of the female, as well as from their direct participation in the birth process. In men, osteoarthritis of the hip joints (coxarthrosis) appears mainly after the age of 65 years.
An important role in the pathogenesis of coxarthrosis plays the natural aging of the body, when the most stressed bone joints begin to collapse.

Also, the disease can be caused by a variety of infectious, traumatic, non-inflammatory diseases, their combination. Initially, osteoarthritis manifests as pain and decreased activity of movements in the pelvic area, but then its consequences become more serious - the affected limb shortens.
Classification of diseases
The types of osteoarthritis of the hip joint depend on the characteristics of its development and the cause of its occurrence. There is often post-traumatic osteoarthritis of the hip joint - it appears after an injury. The classification also includes the following types of osteoarthritis:
- Dysplastic - due to dysplasia that appeared in childhood but was not cured;
- Static - is accompanied by an uneven load in the pelvic area, which occurs with pathologies of the foot, knee, ankle;
- Post-infectious - appears after various inflammatory diseases;
- Primary chronic - develops in the elderly due to aging of the body.
Any type of disease can be called "deforming arthrosis of the hip joint" because the pathology leads to a violation of the shape and appearance of the pelvic articulation of the bone.
In addition, the disease is divided into 3 degrees according to the severity of the changes, the symptoms of which are described below in the text.
Reasons for the development of osteoarthritis
Signs of coxarthrosis can also appear in the absence of obvious preconditions, which is due to natural degenerative processes in the joints. It has a narrow gap while withstanding large and continuous loads, so it is consumed earlier than others. Initially, blood circulation is disturbed in the tissues, so nutrients are distributed to the hyaline cartilage to a lesser extent. Metabolic processes are disturbed, cartilage dries out, cracks are created on it. Further, the articular surfaces get tired quickly, are destroyed - osteoarthritis of the hip joint progresses. Symptoms can appear even faster if the body is affected by a number of provocative factors:
- Any injury;
- Physical work, heavy sports;
- Spinal diseases, including flexion;
- flat feet;
- Arthritis against the background of an infectious process;
- Joint dysplasia transferred to childhood;
- Metabolic diseases;
- Excess weight;
- Rheumatism and other autoimmune pathologies.
Against the background of the influence of such factors, the disease can develop much faster - after 30-40 years.
Symptoms of coxarthrosis
The signs of osteoarthritis of the hip joint depend mainly on its degree. During pathology there are three stages (stages):
- First step. There is pain during physical overload - after a long walk, running, in connection with which there is pain, dull sensation in the pelvic area (pass after a short rest). The pain does not spread to other parts of the foot. Deformative arthrosis of the grade 1 hip joint does not cause changes in gait, the muscles function fully. By the end of the stage, slight restrictions on leg movement may appear;
- The second degree.The pain in osteoarthritis of the hip joint in this case becomes more pronounced. The pain appears with minimal effort, discomfort is present in the evening after a day of work. There is pain at night, at rest. A crack, a feeling of friction in the union. If a person walks for a long time, then the movements of the oscillations can be noticed while walking. It becomes difficult to put on shoes, take the foot sideways;
- Third degree.The work of the pelvic bones is severely impaired (with primary osteoarthritis affecting both joints, with other types, usually only one). The pain in the groin is constant, excruciating, it gives the knee. The thigh muscles are atrophied. The leg becomes shorter, so a person uses crutches and a cane to move.
Later ankylosis occurs, in which movement becomes completely impossible.
Diagnosis of the disease
What is coxarthrosis of the hip joint, what is its degree and how to treat the disease? All problems should be resolved after diagnosis. Although the main method for establishing a diagnosis is radiography, the patient needs consultation with a number of close specialists and tests. This will help to find the cause of the disease and act on it. So coxarthrosis can be caused by osteochondrosis, flat feet, urological and gynecological infections and treating them will help stop the destruction of the bone joint.

In terms of making an accurate diagnosis and determining the degree of osteoarthritis, all the changes are perfectly visualized on an X-ray or CT (MRI) image:
- The first degree is a slight narrowing of the gap, the appearance of marginal osteophytes;
- The second degree - narrowing of the joint space by 50% of the norm, the appearance of osteophytes on the outside and inside of the gap, deformation of the femoral head, often - the presence of inflammatory changes in the tissues near the bone articulation;
- The third degree is a sharp deformity of the joint, the presence of large osteophytes, areas of sclerosis.
Treatment of osteoarthritis
Conservative treatment
Ointments, creams, tablets for osteoarthritis of the thigh help only in the first stage of the disease. Medication can completely restore cartilage and it is important to start therapy at an early stage. Commonly used NSAIDs, corticosteroids, chondroprotectors, hyaluronic acid-based drugs, muscle relaxants. They also practice massage, exercise therapy and therapeutic exercises.
In the second stage, it is necessary to connect physiotherapy and mechanical methods of impact on the joints. These include extractor hood, UHF, magnetotherapy, shock wave therapy, ultrasound, laser, inductotherm, electrophoresis. Folk remedies for hip arthrosis, such as topical medications, are of only secondary importance, and the main method of therapy should be medication.
Be sure to apply a diet for coxarthrosis of the hip joint, it is required to normalize metabolism and improve cartilage nutrition.

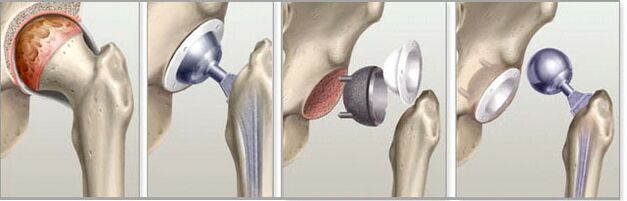
Endoprosthetics for osteoarthritis
The third stage of the disease can only be treated surgically. The patient is recommended joint replacement surgery, or arthroplasty. The surgeon cuts the head of the femur, inserts a metal peg into the incision, over which the artificial head is glued. After the operation, a long rehabilitation and exercise therapy is performed, but then the hip joint will be fully functional and the doctor will be able to answer the patient positively to the question of whether it is possible to sit with osteoarthritis of the thigh. common.
Disease prevention
To prevent osteoarthritis of the thigh, exercise and a healthy lifestyle should come to the fore. It is impossible to overload the joints, but it is necessary to eliminate hypodynamics. Good for walking, swimming, skiing, elliptical trainer. It is also important to lose weight and eat properly.
Prevention of hip arthrosis is also based on early treatment of any bruising, injury affecting the pelvis and spine. In childhood, all congenital joint pathologies should be eliminated as well.
Answers to popular questions
- Who should I contact with arthritis? The question of which doctor treats coxarthrosis of the hip joint does not have a definite answer. Of course, contact with a surgeon, traumatologist or orthopedist is initially recommended, which depends on the skills of the clinic. In specialized centers, an arthrologist deals with pelvic joint problems, but it is not always possible to find such a close specialist.
Depending on the cause of the disease, in the future, in parallel, you will need to apply and undergo treatment under the supervision of a rheumatologist, neurologist, infectologist and a range of other physicians;
- Can arthritis be cured? This disease is chronic and impossible to completely eliminate, especially since the main cause is aging. But if you go to the doctor when there is grade 1 osteoarthritis of the hip joint, you can cure all the existing changes and then prevent rapid progression. In the later stages, it is possible to stop and fix all existing pathological changes and live normally due to regular courses of therapy. Arthroplasty alone can save the joint from osteoarthritis, but there are also a number of disadvantages - from the need for periodic prosthesis replacement to postoperative complications - pain, thrombosis, infection;
- When are local therapies sufficient and in which cases can a visit to the doctor be avoided? Any ointment can slightly improve blood microcirculation in the joint area, and also relieve pain, but has no therapeutic effect. In addition, this node is located very deep, which makes the penetration of active substances difficult. Therefore, it is necessary to consult a doctor at any stage of the disease, regardless of the severity of the manifestations. Only at an early stage can the disease be stopped with "little blood" without surgery.
Osteoarthritis of the hip joint is an incapacitating pathology that makes a person crippled, preventing him from walking.
The only way to prevent the development of such problems is to start conservative therapy in stages 1-2 of the disease, not forgetting to take regular and complete courses.


















