
Osteoarthritis of the knee joint is a specific disease that has a destructive effect on the cartilage of the knee joint.
When such a disease appears, doctors notice serious disturbances in blood circulation processes in bone vessels, as a result of which deformation and destruction of cartilage tissue occurs, the person feels severe pain that limits any movement of the legs and knees, and notices swelling and changes in the appearance of the knees.
To prevent the development of severe consequences of gonarthrosis (deformation of limbs and ankylosis - immobilization of the joint), when only joint replacement surgery can help the patient, the disease must be identified and treated immediately.Moreover, treat it not independently with folk methods and advertised means, but under the supervision of qualified doctors.
What are the reasons?
Mechanisms of arthrosis in medicine are usually divided into:
- PRIMARY- which occurs in old age from the natural aging of body tissues and against the background of several factors that provoke this disease, such as obesity (10% of cases), heredity, increased stress throughout life.
- Medium- accounts for 30% of all cases of knee arthrosis;it usually manifests after an injury, a fracture of the tibia, rupture of ligaments or damage to the meniscus.Moreover, with such arthrosis of the knee joint, the symptoms of the disease in most cases appear after 3-4 years, but after a serious injury it is possible even after 2-3 months.
In 50-60% of cases, the cause of arthrosis of the knee joint is spasm of the muscles of the front surface of the thigh.
What happens to the knee joint with osteoarthritis?
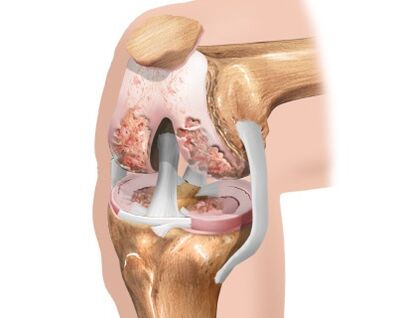
With regular excessive loads, genetic predisposition, metabolic disorders in the body, spasms and prolonged muscle injuries, the knee cartilage loses its softness and begins to thin.The soft sliding of the articulated bones is replaced by strong friction and the first degree of gonarthrosis develops, in which the cartilage loses its shock-absorbing properties.
The degradation process continues to progress and poor shock absorption leads to the flattening of bone surfaces with the formation of osteophytes in the form of bone growths.In this case, the disease already has a second degree and is accompanied by degeneration of the synovial membrane and articular capsule.The lack of pumping and movement atrophies the structure of the knee joint, the consistency of the knee fluid becomes more viscous, the process of cartilage nutrition is disrupted, which leads to an even greater deterioration of the patient's condition.
Cartilage thinning leads to a reduction in the distance between articulated bones by up to 80%.During walking, due to abnormal friction and the lack of a shock absorber, the destructive processes in the joints increase rapidly, this quickly leads to the development of the third degree of arthrosis with pronounced symptoms:
- Pain when moving, especially when going up or down stairs.
- Pain both during exercise and at rest, morning stiffness.
- The patient begins to limp, trying to save the injured joint.
- Severe cases of the disease require the use of crutches or a cane.
The third degree of arthrosis of the knee joint is characterized by an almost complete absence of cartilage tissue, which leads to a decrease in the mobility of the joint to a minimum.Therefore, no magic method, super drugs or ointments can restore the worn cartilage tissue, and given the degree of bone deformation, the normal functioning of the joint is impossible.In this case, only surgery can help.
Stages of arthrosis
As arthrosis progresses, the following stages or degrees are distinguished:
- The initial stage, or stage 1, is often called compensated, since there are still no pronounced clinical signs of the pathology.The patient may feel discomfort in the knees after physical activity, which disappears quickly after rest;nodes are still fully functional.
- With grade 2 arthrosis, undercompensated, the symptoms of the disease intensify.A pronounced pain syndrome is formed, which, however, is relieved by anesthetic ointments and gels used topically.Motor activity is impaired and joint instability appears.In the vast majority of cases, patients at this stage turn to doctors.
- The 3rd degree, decompensated, can also be called deforming.The knee joint is twisted, unstable, immobile and completely non-functional.The pain syndrome is persistent and requires serious medical intervention.To unload the joint and move, a person needs a cane.
First symptoms and signs
Depending on the severity of the symptoms, the development of the disease is divided into 3 stages.Symptoms of the early development of gonarthrosis vary greatly and are not specific.
In the first stage of the pathology, the following symptoms are possible:
- knee pain when sitting or walking up stairs;
- joint pain after exercise or prolonged cold;
- the knee may hurt at the end of the day or in the morning;
- stiffness and pain in the morning go away after daily work.
Then the characteristic symptoms of stages 2 and 3 appear (in ascending order):
- the pain becomes acute and prolonged;
- swelling in the joint area;
- fluid may appear in the joints;
- between the articular surfaces, compression of cartilage particles, meniscus, synovial villi is possible, as a result of which sharp immobility occurs (it can also pass suddenly);
- it is difficult to step on your feet;
- joint immobility develops.
The consequences
If left untreated, the following complications of knee arthrosis may develop:
- Deformation of joints.In fact, joint deformity is most likely not a complication, but in the final stage of the disease.
- Infection in a joint.Infection usually occurs due to microtrauma.They can be considered small cracks in the cartilage tissue.Pathogenic microorganisms enter the joint through the flow of blood or lymph from other areas.This often happens after infectious diseases.
- Dislocations and fractures.These complications are explained by dysfunction of the knee joint.With arthrosis, there is no uniform distribution of the load from the femur to the bones of the lower leg.The ligaments that normally strengthen the joint also weaken.Because of this, at a certain moment (even during normal walking) the bones of the lower part of the leg can be subjected to excessive stress, which will lead to a fracture or displacement.To avoid this, people with severe structural and functional damage to the knee joint must move with the help of a crutch or cane.
- Ankylosis.Ankylosis is the fusion of two bones where a joint once existed.This complication is perhaps the most serious, as the key simply disappears.The tibia and femur are gradually fused, and the tibia is fixed in one position.Movement, of course, is impossible.
Diagnosing
To diagnose gonarthrosis use:
- blood tests (general and biochemical);
- radiography;
- arthroscopy;
- Ultrasound;
- MRI.
The most important diagnostic method for confirming the diagnosis of gonarthrosis is radiography.Although it is not possible to examine the initial stages of the disease and the condition of the cartilage tissue on x-rays, however, the bone changes of stages 2 and 3 are clearly visible.This:
- narrow common space;
- marginal spines located along the contour of the bones, the edges of the patella - osteophytes;
- changes in the periosteum;
- changing the height of one of the condyle and others.
However, changes can be examined in more detail using arthroscopy.
Ultrasound and MRI help detect changes in the soft tissues of the knee joint during early arthrosis.These methods also provide a good indication of the condition of cartilage tissue, synovium and fluid.
How to treat arthrosis?
Treatment for osteoarthritis of the knee joint is long and sometimes painful.The duration is due to the fact that once the disease has appeared, it will constantly remind itself as long as the person lives.
Thus, to properly treat gonarthrosis, a fairly strong financial foundation and discipline is required.An important role is played by how seriously the patient takes the treatment, since often, in order to reduce the frequency of exacerbations of the disease, the patient is forced to change his daily activity, favorite profession, engage in joint development, quit smoking and drinking alcoholic beverages.
There are three main stages in the treatment of deforming arthrosis of the knee joint.
The first stage of treatment includes:
- communicating with patients the nature of their disease, risk factors and secondary prevention measures;
- daily gymnastics with stretching elements;
- contrast shower;
- swimming in the pool 2-3 times a week;
- weight loss.
The second stage of treatment includes:
- external fixation of the joint using calipers, bandages, elastic bandages and orthoses;
- the use of ointments and creams based on non-steroidal anti-inflammatory drugs to relieve inflammation and pain;
- the use of drugs from the group of chondroprotectors to reduce the rate of cartilage destruction.
The third stage of treatment includes:
- Course of use of oral NSAIDs;
- intra-articular injections with anti-inflammatory hormonal drugs;
- additional use of drugs with a pronounced analgesic effect;
- surgical replacement of a diseased joint with an implant.
Along with drug treatment, modern medicine uses methods such as:
- Kinesitherapy.In this case, the treatment of arthrosis of the knee joint is carried out using special exercises.The load is selected in accordance with the degree of development of the disease and the physical ability of the individual patient.
- Ozone therapy.This is an effect on an injured knee joint using ozone.With this method of physiotherapeutic treatment, the substance can be administered by injection or used externally.
- dietary supplement.Biologically active supplements are a worthy alternative to other drugs.
- Homeopathy.It involves taking medications in small doses.The course of treatment lasts only a few weeks, but during this time, provided that the drugs are chosen correctly, blood circulation and normal nutrition of cartilage tissue cells are fully restored.
- exerciseallows you to improve blood circulation in the knee joint, restore the elasticity of the ligaments, improve the nutrition of cartilage tissue cells and promote its restoration.
Drug treatment
All medications used in the treatment of gonarthrosis can be divided into those that help eliminate the main symptoms of the disease and those that restore the function of the knee joint and prevent the progression of the pathology.The first type of drugs includes non-steroidal anti-inflammatory drugs and hormonal drugs.The second group includes chondroprotectors and hyaluronic acid.
Nonsteroidal anti-inflammatory drugs
Drug treatment of arthrosis begins with the elimination of pain.They are the ones that cause the greatest moral and physical suffering in patients and lead to the loss of the ability to work.Nonsteroidal anti-inflammatory drugs (NSAIDs) have worked well among pain relievers.
Medicines can be used in two ways - topically or orally (in tablets).Topical (preferred) treatments often include patches, ointments, or gels.The analgesic effect, as a rule, occurs on days 3-4, and its maximum develops on days 7-10.
The course of treatment with non-steroidal drugs should be limited to 10-14 days.NSAIDs have a limited range of use and are used with great caution in the treatment of elderly patients.
Hormonal drugs
In cases where NSAID treatment is not sufficient and the disease continues to progress, the doctor may prescribe hormonal injections.They belong to the tools of "heavy artillery" and help to quickly eliminate pain, relieve inflammation and swelling of the surrounding tissues.
Due to the large number of side effects, hormonal drugs are prescribed in short courses, only during the acute period of the disease, when inflammatory fluid accumulates in the joint cavity.The drug is administered in the common space no more than once in 10 days.
Chondroprotectors
To prevent further destruction of the cartilage surfaces of the joint, chondroprotectors are prescribed.
These drugs also help reduce pain and reduce signs of inflammation in the surrounding soft tissues.In addition, chondroprotectors slow down the destruction of joint tissues and stabilize the disease due to their absorbing and lubricating functions.Chondroprotectors improve cartilage nutrition, normalize the composition and properties of intra-articular fluid and protect pain receptors from excessive irritation.
Hyaluronic acid
Hyaluronic acid is called a liquid intra-articular fluid prosthesis.In its properties, it is similar to the natural synovial (intra-articular) fluid, which nourishes the cartilage tissue and protects the knee joint during movements.
Hyaluronic acid preparations are injected into the joints, thus creating a thin protective layer that prevents the cartilage surfaces from rubbing against each other.Injections are performed only after the acute phase of the disease has passed.
Exercise therapy and exercises for osteoarthritis
Physical exercises help restore joint function and strengthen it.They must be carried out slowly and carefully so as not to cause strain and not exceed the permissible load.
The following exercises are considered the most effective:
- Slowly raise your straight legs one at a time while lying on your stomach.This exercise uses the thigh and calf muscles.The load must not be allowed to transfer to the rear.You shouldn't raise your legs too high either.The main thing is to strain your muscles at the top point;
- This exercise is similar to the first one, only now you have to lift the leg with the knee bent.At the top point, the thigh muscles should be further tensed.The exercise should be performed the same number of times on each leg;
- Lying on the floor (on your stomach), lift your straight legs up and then spread and bring them together.This exercise requires strong and trained abdominal muscles, so it is not suitable for all patients.In addition, doing it can increase blood pressure.For patients suffering from hypertension or other diseases of the cardiovascular system, it is better to avoid it;
- To perform the next exercise, you need to lie on your side, bend the leg lying on the floor at the knee and slowly raise the other and keep it at the top point.It is important that the angle when performing on each leg is the same;
- For this exercise you will need a chair.Sitting on it, the legs are straightened one by one, lifted up and held for the maximum possible time in a straightened position;
- It is helpful to stand on your toes while holding the back of a chair or bed.As with other exercises, you need to stay at the top point for a few seconds and also strain the leg muscles;
- Smooth movement from toe to heel allows you to activate blood circulation in the lower extremities.Such movements should be performed alternately: while one leg stands on the toe, the other on the heel and vice versa.All movements should be smooth;
- Leaning on the back of a chair or bed, stand on your heels for one minute, lifting your toes up.If you cannot stay in this position for the specified time, you should start with less, gradually increasing it;
- A massage performed in a standing position.The legs should be rubbed with powerful movements directed from the knee to the thigh.It is necessary to finish the massage by stroking the skin.
The doctor will conduct several sessions in the office and show the basic techniques so that the patient can massage the problematic knee himself.Competent actions improve the condition of the damaged area.
Massage and self-massage
Perform self-massage with your palm, palm edge, fingertips or fist.Act gently on the injured knee, keep strong pressure on the affected area: strong blows, blows, active stirring of the tissues often worsen the condition.
Basic techniques:
- the first stage is a light stroke clockwise, the second stage is a circular movement in the opposite direction;
- Press a palm on the injured knee, touch lightly with the fingertips of the other hand;
- keep the initial palm position, tapping not with your fingers, but with the edge of your palm;
- gently hit the knee in a circle, gradually increase the pressure (but in moderation);
- During therapy, massage the affected area twice a day for 10-15 minutes.For preventive purposes, it is enough to do a light massage once every 7 days.
Before the procedure, apply an ointment or gel with an anti-inflammatory effect to the injured knee.
Physiotherapy treatment
All physiotherapy methods can be divided into several groups:
- Pain reduction;
- Reduction of inflammation;
- Restoring nutrition to the joints and accelerating the restoration of joint function.
The doctor can determine what kind of treatment the patient needs based on the existing symptoms and co-morbidities.
Surgery for arthrosis
Surgical treatment refers to radical methods that partially or completely restore the functioning of the knee joint.Surgical treatment methods differ from each other in the degree of intervention in the affected joint.
- Arthroscopyrefers to the mildest methods of surgical treatment.This technique is less traumatic and can be used as a therapeutic measure even in the early stages of arthrosis.Its main purpose is to prolong the life of the damaged joint.Arthroscopy is performed using an endoscope - a flexible probe with a camera at the end.Small holes are made in the knee joint, through which the endoscope and auxiliary instruments are inserted.During the operation, damaged areas of tissue that cause pain are removed.The operation is more suitable for young people and, if necessary, can be repeated several times.
- Endoprostheticsrefers to the most radical surgical techniques.In this case, the complete restoration of joint function occurs by replacing the entire knee joint or part of it with an implant.This method is the best alternative to the previously existing technique - arthrodesis (complete immobilization of the damaged joint).Currently, endoprosthesis replacement gives up to 90% positive results and significantly improves the quality of life of patients.
- OsteotomyIt is used when significant deformations have developed in the joint and the function of the joint is clearly impaired.Osteotomy involves creating an artificial bone fracture at a pre-planned location.The bone pieces are then aligned in the correct, physiological position and allowed to grow together.Sometimes during surgery, artificial fixators of bone fragments can be used, which contribute to a more stable position of the bone.
Folk remedies
Traditional medicine will also help you.The use of various lotions to relieve swelling and pain has long been practiced by many patients.Here are some useful recipes:
- Burdock leaves.Take 5 burdock leaves and hold them over boiling water to steam them.Rub the injured knee with vegetable oil and apply the steamed leaves.Wrap the leg in cling film and a warm scarf.Leave the lotion on for several hours.
- Cabbage leaf lotion.It is made from fresh cabbage leaves soaked in May honey and applied to the feet.The therapeutic effect is strengthened by insulation made of woolen fabric or plastic film.This product is suitable for people of all age groups.
- Eggshells, kefir.Grind the shells of 2 eggs and mix with 1 spoon of kefir.Apply the mixture to your knee, wrap it in a cloth and cling film and lie down under a blanket.Leave it like this for several hours, then rinse the composition with water.This treatment can be used every day.
- Horseradish compress.According to this popular recipe, to improve the medicinal properties of horseradish, it is recommended to first press and boil it.Then it should be applied to the affected area.
- Turpentine– an excellent warming agent for sore joints.The knee is rubbed with turpentine before going to bed and tied with a woolen scarf.Already after the first procedure, the patient experiences considerable relief.The course of treatment is chosen individually for each person.
diets
The therapeutic diet includes avoiding or minimal consumption of canned, smoked and fried foods (to suppress appetite).To restore the damaged cartilage, it is necessary to provide the body with complex carbohydrates (porridge, integral products).Juices (carrots, beets, apples) should also be included in the diet.They will remove toxins from the body and reduce the impact of inflammatory processes.
The diet should include fish and aspic, which act as a type of chondroprotector and help create new cartilage.It is worth remembering that you cannot prescribe a diet for yourself - only a nutritionist (diet specialist) can choose the best option.
Sample menu:
- Breakfast: oatmeal with water without butter or sugar, fruit juice, boiled egg;
- Second breakfast: a glass of low-fat natural yogurt;
- Lunch: steamed meat or fish, boiled vegetables, tea without sugar;
- Afternoon snack: cottage cheese casserole with nuts, a glass of fruit juice;
- Dinner: vegetable salad, apple, tea without sugar;
- Second dinner: a glass of low-fat kefir.
Preventing
Prevention of joint diseases:
- dose the load on the legs during active sports;
- create a diet that includes foods and dishes containing calcium, magnesium, gelatin;
- if the work involves lifting or moving heavy objects, follow safety rules and do not carry loads that exceed a certain limit;
- Do self-massage regularly to prevent arthrosis, especially with constant stress on the legs;
- eat right, limit "harmful" foods;
- body weight control (excess weight means additional stress on the joints);
- Have regular examinations and treat acute and chronic diseases.
PREDICTION
Provided that arthrosis of the knee joint is diagnosed in the early stages, the cause of the pathological process is eliminated and adequate treatment is provided, the prognosis is favorable.The therapy offered makes it possible to achieve long-term remission, but the treatment is usually lifelong.
In the absence of the necessary treatment, as well as when the patient does not follow the doctor's instructions, arthrosis of the knee joint becomes a cause of disability.


















