Osteoarthritis of the knee is very common in the elderly, especially in women. It is also diagnosed in young people. This disease significantly reduces the quality of life and, if not treated properly, can lead to disability.
How to recognize osteoarthritis? What are the causes of this disease? How to cure it?
signs
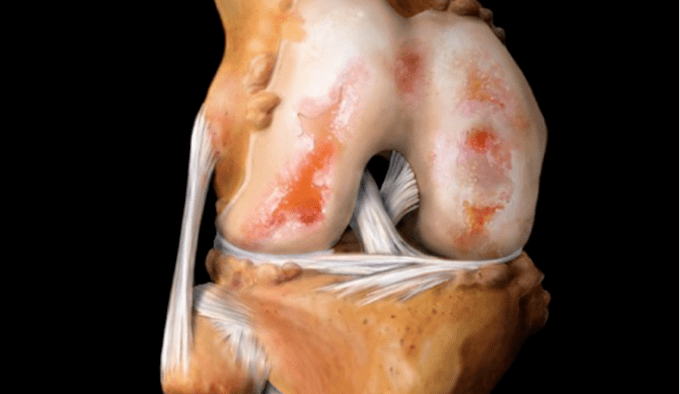
Osteoarthritis is an injury to the hyaline cartilage of the ankle. This cartilage is gradually destroyed. First, its structure, density changes, then it becomes thinner. In severe cases, cartilage may be completely absent.
There is always a fairly strong load on the knee joint because it is one of the major structural elements of the lower limbs. Therefore, signs of osteoarthritis of the knee joint are visible even with minor joint damage.
In osteoarthritis of the knee, the symptoms are accompanied by pain and gradual loss of knee function.
There are three stages in the development of the disease. Each of them has characteristic symptoms and requires proper treatment.
The first phase
The first stage in different people can be of different durations. In some, the changes in the joints progress quickly and after a few months the disease passes to the next stage. In others, dystrophy of cartilage tissue structure occurs slowly, years pass before new symptoms appear.
Signs of the first stage of knee osteoarthritis:
- Persistent pain in one or both knees. It usually happens in the morning, when you try to take the first steps, during a long stay in a standing position or when you walk up or down stairs. The reason for the appearance of a particularly pronounced pain is the descent down the stairs. There is no pain at rest.
- There are frequent complaints of a slight feeling of stiffness with intense movement in the wrist area. But changes in the amplitudes of the movements are not noticeable.
- There may be slight deformation due to fluid in the ankle cavity, but the bone has not changed.
All of these symptoms indicate the need to see a doctor. If you start treatment at this stage, there is the possibility not only to stop the process, but also to start the recovery processes in some parts of the cartilage.
Second phase
If you do not seek medical help, the disease passes to the next, second stage. At the same time, the old symptoms worsen and additional complaints appear.
Signs that the arthrosis has progressed to the second stage:
- The pain intensifies. Occurs with every foot movement. With prolonged walking, lifting heavy objects, the discomfort is particularly pronounced. At rest, the pain gradually decreases.
- When you move, there is pain and a crack from the affected joint.
- The range of possible movements begins to decrease, which can cause discomfort. When a person tries to bend the leg at the knee until it stops, he either fails, or the bending causes a sharp pain.
- During the examination, the doctor notices small changes in the shape of the wrist. If an x-ray is done, it will be seen that the joint space is too narrow and growths are formed at the bony edges.
- A large amount of fluid can accumulate in the ankle cavity. This can be detected during diagnostic procedures and during routine examination.
Most often, patients go to the doctor at this stage. In this situation, it is very difficult to achieve a significant recovery, but some positive changes are possible.
The third stage

The third stage occurs with severe cartilage destruction and is more severe. Complaints and examination results of a patient with stage III osteoarthritis:
- Severe, almost constant pain in the affected joint. When you try to move, it intensifies. At rest, even in the supine position, the pain does not go away, so there are problems with sleep.
- Movement in the joints is very limited.
- Often the knee "rises" in a slightly bent position. This affects the shape of the foot and the patient's gait.
- Examination shows marked deformity of the ankle and bones.
- X-ray image shows the absence of cartilage in many areas of the articular surface, bone sclerosis. The joint space is significantly narrowed, a large number of osteophytes are found.
Managing these patients is particularly difficult. You may also need surgery.
reason
The causes of osteoarthritis of the knee joint are very different. Very rarely, a person who has been diagnosed with this disease has only one factor that has caused the pathological process. In most cases, changes in cartilage are due to a variety of reasons. The more risk factors, the more intense the destruction and loss of functionality.
Most often, arthritis is provoked by such characteristics of the body and circumstances:
- age-related changes in the structure of the musculoskeletal system;
- knee injuries, as well as surgeries in which joint damage can occur;
- too much load on the lower limbs;
- congenital abnormalities of the musculoskeletal system or metabolic processes;
- inflammatory processes of various etiologies in the knee area.
Let's take a closer look at these groups of causes.
Age changes
Most often, knee osteoarthritis develops after 40 years. This is due to the fact that at this age and older, the structure of bone and cartilage tissue becomes more fragile, their resistance to stress decreases. Therefore, even long walks can be difficult to tolerate by the lower limb joints.
Changes in the musculoskeletal system in women during menopause are particularly pronounced.
During this period, the level of estrogen, which previously protected the bones from calcium loss, gradually decreases, they become more vulnerable.
Injuries and surgeries
In young people, osteoarthritis can occur due to trauma. It could be a broken leg, a dislocated knee, a broken ligament, or a severe bruise. The longer the time from the moment of injury to the right help is given, the higher the risk of complications and the appearance of osteoarthritis in the near future. Therefore, even with minor knee injuries, you should go to the hospital.
There is also a high risk of developing osteoarthritis after surgery in the knee area. Meniscus removal is especially dangerous. After such an operation, osteoarthritis appears in approximately 80% of patients.
Traumatic osteoarthritis usually develops quickly. Therefore, in such cases, surgical intervention may be necessary.
Overload
Excessive stress on the knees is observed in athletes who professionally engage in sports related to running, jumping, lifting weights. The older a person gets, the more carefully he should choose the options for physical activity in training. Particularly dangerous for the knees are squats, sudden movements and running on paved paths.
Excessive stress on the ankle joints is typical for people suffering from obesity. Then its own weight creates excess pressure on the cartilage and bones, which leads to their rapid consumption.
Congenital pathologies
In case there are pathologies in the musculoskeletal system and metabolic processes, this can also affect the knee joints.
Congenital pathological conditions that imply a high risk of developing osteoarthritis:
- knee joint abnormalities;
- flat feet;
- disorders of salt metabolism;
- ligament weakness.
If you are aware of such problems, it is important to be especially attentive to knee pain, not to ignore it, and try to work closely with doctors.
Inflammatory phenomena
With arthritis of various etiologies, a large amount of fluid can accumulate in the joints. This leads to the fact that blood circulation is disturbed, nutrients do not reach the bones and cartilage, the structure of cartilage tissue is destroyed. As a result, secondary osteoarthritis develops.
No less dangerous are the inflammatory processes in the vessels of the legs that nourish the knee. When they are blocked by a thrombus, the blood supply is significantly reduced, which leads to degenerative processes in the cartilage.
Treatment
Therapy is prescribed taking into account the degree of development of the disease, its causes and the general condition of the body. Principles of osteoarthritis treatment:
- pain reduction;
- improved cartilage supply of nutrients;
- stimulation of recovery processes;
- an increase in joint space to reduce pressure on the damaged cartilage;
- strengthening and restoring the functions of the muscles surrounding the joint;
- maximum recovery of motor skills.
There are several treatment options for osteoarthritis of the knee. They usually involve a complex of therapeutic procedures.
What can be prescribed to treat this disease:
- Therapeutic exercises. They are selected by the orthopedist for each patient separately. If you try to create a complex yourself, get involved in pain, joint damage will progress.
- Diet.
- Surgery, prosthesis.
- Drug treatment: non-steroidal anti-inflammatory drugs (tablets or injections), painkillers, chondroprotectors, injection of glucocorticoids or hyaluronic acid preparations into the joints.
- Additional procedures: hirudotherapy, massage, magnetotherapy, paraffin or ozocer heat, electrophoresis, manual therapy and others.
If you have joint pain, you should see a doctor. Timely treatment is the key to successful treatment.


















